Day :
- Sessions: Childhood Obesity | Bariatric surgery | Childhood Obesity Prevention | Behavioral & Environmental Factors | Exercise & Kinesiology | Thyroid and Obesity | Bariatric surgery for obesity and metabolic disorder | Obesity

Chair
Jovanna Dahlgren
University of Gothenburg, Sweden

Co-Chair
Theresa Loomis
University of Medicine and Dentistry of New Jersey, USA
Session Introduction
Beverly Copeland
Prairie View A&M University, USA
Title: A Foods and Nutrient Comparison Study of Meals Eaten at Home vs Meals Eaten at Head Start Centers in Washington DC, USA
Time : 11:40-12:05

Biography:
Beverly Copeland has her expertise in childhood obesity working in low-income and underserved populations. She seeks to find solutions to the prevention and treatment of childhood obesity. Dr. Copeland is a registered and licensed dietitian with the skill set needed to understand and develop tailored nutrition intervention programs to combat childhood obesity. She continues to work with caregivers, teachers, and other stakeholders who are interested in seeing childhood obesity on a downward trajectory. She is currently working on research to analyze and evaluate meals served in State-Registered Private Childcare Settings. This information will be used to determine the adequacy of meals served to children against the 2015-2020 Dietary Guidelines. Dr. Copeland is currently an Assistant Professor in the Department of Agriculture and Human Ecology at Prairie View A&M University. She previously served in the department for two and half years as the Director of the Didactic Program in Dietetics.
Abstract:
The purpose of this research was to investigate the food energy and nutrient intake, and adequacy of meals served at Head Start centers versus meals consumed at home among Head Start Children. A cross-sectional descriptive survey research design was utilized. A convenience sample of 195 Head Start child and caregiver pairs was recruited from two Head Start sites within the District of Columbia (DC). Weight and height were measured and used to calculate BMI. The Centers for Disease Control and Prevention (CDC) BMI for age and gender growth charts were used to evaluate BMI levels. Dietary intakes were collected using the 24-hour food recall method, and Head Start center menus were analyzed using Nutritionist Pro Software (Axxya Systems, Redmond, WA). Data analysis was conducted using the Statistical Package for the Social Sciences (SPSS) version 19 (IBM SPSS Inc., Chicago, IL). Results of the study showed no significant difference in total calorie intakes between the overweight/obese children and normal weight children who consumed meals both at home and at Head Start centers. However, in both overweight/obese and normal weight children who consumed meals totally at home, lower nutrient intakes were noted when compared to recommended levels. It was concluded that Head Start children who consumed meals both at school and home on the day of the recall, had higher intakes of food energy and were more likely to meet recommended nutrient intakes than Head Start children who did not consume any portion of their meals at school.
Kathleen Border
D’Youville College ,USA
Title: An evaluation of a pilot Farm to School program: Student knowledge and awareness
Time : 12:05-12:30

Biography:
Kathleen Border is a nutrition education professional with over twenty years of experience designing and implementing education programs for diverse audiences. She is an advocate for bringing nutrition education programs to underserved communities throughout her career in dietetics. Her experience in community nutrition and higher education has led her to collaborate with stakeholders to support healthy eating initiatives in schools. Professor Border is an academic leader with proven success in designing and meeting national accreditation standards. She has held several leadership positions within the Academy of Nutrition and Dietetics. She currently serves as an Assistant Professor of Dietetics at D’Youville College, Buffalo, New York.
Abstract:
Statement of the Problem: The percentage of children with obesity in the United States has more than tripled since the 1970s. Today, about one in five school-aged children (ages 6–19) has obesity. School based interventions to promote healthy eating and prevent obesity are a natural fit. Farm to School is a voluntary program through which schools can purchase and highlight locally produced, farm-fresh foods. The program also promotes nutrition-based curriculum and experiential learning opportunities such as farm visits and school garden-based learning. This study evaluated a Farm to School pilot program in a large urban school district to determine students’ awareness of the program at their school and if they could identify benefits of consuming locally grown produce. Methodology & Theoretical Orientation: A quasi-experimental study design was used. Students in a large urban school district participated in two nutrition lessons which focused on 1) awareness of the Farm to School program and 2) benefits of eating locally grown foods. A pre and post-test was used to evaluate change in awareness and knowledge. The Whole School, Whole Community, Whole Child (WSCC) framework was applied which combined elements of the traditional coordinated school health approach and the whole child framework. Findings: The sample consisted of 4th grade students (n=290) enrolled in ten schools within a large urban school district. All ten schools were part of a Farm to School pilot program. After the intervention, a significant difference (p< .001) was noted in program awareness. Students demonstrated an increased knowledge of locally grown produce after the nutrition intervention, specifically apples (p=.009), pears (p=.001), broccoli (p=.031), and cauliflower (p=.005). Additionally, students identified benefits of consuming locally grown produce, specifically that the food tastes great (p=.011) and will support local farms (p=.004). Conclusion & Significance: This study found that the nutrition education component of the Farm to School program increases 1) knowledge of locally grown foods, 2) benefits of consuming locally grown foods and 3) awareness of the Farm to School program within their school. Farm to School programs enhance student knowledge of consuming fruits and vegetables. Future research needs to be conducted to determine changes in eating behaviors based on participation in the Farm to School program.

Cláudia Araújo da Rocha Benevides
Federal University of Pará ,Brazil
Title: Influence of parents on the development of Childhood Obesity
Time : 12:30-12:55

Biography:
Cláudia Araújo da Rocha Benevides has completed her Graduate of Medicine in 2004 from Federal University of Para (Brazil), in 2013 her post graduate program in Nutrology from Faculty of Medical Sciences of the Holy House of São Paulo. She is Master Business Administration in Health Management. She has published a lot of papers in Medical Journals and has been treating patients at the office in her area of expertise since then.
Abstract:
Statement of the Problem: Childhood obesity has been growing in the world in alarming numbers, Brazil is among the countries where this growth calls attention, in the last 20 years the number of obese among children 5 and 9 years has increased more than 4 times. The literature on infant nutrition points out that the development of food preferences that define the pattern of feeding in childhood is determined by the family. Methology & Theoretical Orientation: Data analysis of questionnaire applied to one of the parents of 70 children between 2 years and 8 years. The classification of the nutritional status of the children was carried out applying the curves of Body Mass Index (BMI) for the age of the World Health Organization. The Chi-Square statistical test was used. Findings: Of the 70 children who participated in the study, 51.4% were eutrophic, 21.4% were obese, 18.6% were overweight and 8.6% were lean. Among those classified as overweight and obese in 85.7% of the cases at least one of the parents were obese or overweight by the BMI (p = 0.0483). Regarding the total sample of participants, when parents were asked if they had offered children candies before age 2, 81.4% had offered. Of these, 10% assumed that children consuming sweets practically every day, while 38.6% stated they only allowed consumption eventually in cases of celebrations. Conclusion & Significance: In this study we can see that the vast majority of overweight children had at least one parent in the same condition, it is of fundamental importance that parents are aware that their habits directly influence the eating behavior of their children and that the high supply of candies, foods of known low nutritional value, early in life may be determinant for the creation of taste buds and food preferences that are not adequate in this and that have contributed to the development of obesity in childhood.
Biography:
Abstract:
Marc Schiesser
Obesity Center Kantonsspital St. Gallen, ,Swaziland
Title: Bariatric surgery in adolescents and young patients: What is the better option gastric sleeve resection or gastric bypass?
Time : 13:40-14:05

Biography:
Marc Schiesser has long standing expertise in bariatric surgery and is a cofounding member of the obesity center in St. Gallen, which has brought the adult obesity center together with the obesity unit of the childrens hospital in 2013. This merge has resulted in a close collaboration and share of expertise for obese adolescents and children. The surgical therapy is one of the therapeutic options, which has been successfully established in our center. As a board member of the swiss society for the study of morbid obesity and metabolic disorders he has been involved with the establishment of the swiss guidelines for bariatric surgery in adolescents and childrens.
Abstract:
Background and objectives:
The prevalence of obesity in adolescents and young patients is steadily increasing and bariatric surgery has become a standard treatment for selected patients. Sleeve gastrectomy (SG) and gastric bypass (GB) are the standard procedures for adults. However, it remains unclear which operation should be offered to adolescents and young patients. Therefore, we compared the results of these procedures in this population.
Methods:
All patients undergoing bariatric surgery <26 years were prospectively assessed between 01/2013 and 01/2017. The choice of the operation technique was based on the interdisciplinary meeting. The primary end point was weight loss at one year. Secondary end points were perioperative complications (Dindo classification) and reoperation rate.
Results:
We assessed 104 patients with a mean age of 22.7 years (range 17.2-25.8 years). The mean follow up was 547 days. 87 patients underwent GB surgery and 17 had SG. The mean BMI was 44.9kg/m2 at the time of operation. Weight loss was similar in both groups at one year with a BMI of 29.5kg/m2 in the bypass versus 31.9kg/m2 in the sleeve group (NS). The perioperative complication rate (grade 2 or less) was 4.5% (4/87) in the bypass and 11.8% (2/17) in the sleeve group (NS). Six (6.8%) patients underwent laparoscopy for internal hernia in the GB group. No reoperation was observed in the SG patients.
Conclusion:
GB and SG in adolescents and young patients are both safe and effective. We observed a higher rate of reoperations in the GB group, mainly due to internal hernia.
Vaclav Bunc
Sport Charles University, Prague Czech Republic
Title: Effect of exercise on body composition in children differing in body mass
Time : 14:05-14:30

Biography:
Václav Bunc has his expertise in application of mathematical methods and models in PE and sport, using of biocybernetics by evaluation of physical fitness, exercise physiology, functional and physical testing in laboratory and field, body composition, BIA methods, moving regimes for prevention in cardiac patients. He is the first author more than 400 items in scientific Journals, more than 150 abroad, practically the same number of publications as co-author. s responsive to all stakeholders and has a different way of focusing.
Abstract:
Statement of the Problem: Childhood overweight and obesity are a worldwide problem. Childhood overweight and obesity has major consequences in all stages of life; it is associated with co-morbidities such as glucose intolerance, diabetes, metabolic syndrome and other cardiovascular risks factors at young adulthood. Alongside a range of health problems associated with increased body mass (BM), overweight or obesity is an important limiting factor for realization of PE and qualitative life style. Methods :In study we assess the effect of exercise in children differing in BM. Study was carried out in 98 children with normal BM (age=12.4 ±2.2 years; BM=48.0±3.6 kg; height=157.0±4.8 cm), 68 overweight (12.1±2.0; 61.6±3.0; 157.7±4.5) and 59 obese (12.7±2.6; 71.2±3.8; 155.1±4.2). The mean energy content of exercise/week in normal BM children was 1920 ± 310 kcal, in overweight 1990 ± 230 kcal, and in obese 2260 ± 290 kcal. The exercise was based on walking (82.0±3.1 %) of all movement activities. Results: Relative changes after the imposed movement intervention in %BF ranged from 15.4 in obese to 16.6% in normal BM and in VO2peak from 13.9 in normal BM to 15.7% in obese. In our children are absolute changes in somatic and functional parameters like a result of imposed exercise based on walking substantively and statistically significant. On the contrary, differences in relative terms are insignificant. Conclusions: We may conclude that similar exercise program may invoke the similar BC and functional performance changes in pre-pubertal children differing in BM.
Elisabet Wentz
University of Gothenburg ,Sweden
Title: Eating and Neurodevelopmental Disorders in a Clinical Sample of Children and Adolescents with Obesity
Time : 14:30-14:55

Biography:
Elisabet Wentz is the manager of Gillberg Neuropsychiatry Centre, university lecturer (the Birgit Olsson lectureship), Associate Professor of child and adolescent psychiatry, University Hospital senior consultant at Child Neuropsychiatry Clinic, Queen Silvia Children´s University Hospital, and licensed as a specialist in child and adolescent psychiatry and psychiatry. Her PhD thesis from 2000 was titled "Ten-year outcome of anorexia nervosa with teenage onset". Her current research includes, but is not limited to, longitudinal follow-up studies of anorexia nervosa, the correlation between obesity, neuropsychiatry and eating disorders, eating disorders within the autism spectrum, non-pharmacological interventions (including IT interventions) in cases of neuropsychiatric disabilities, as well as neuropsychiatric comorbidity in cases of various syndromes. She has had post doc position at St. George’s Hospital Medical School, London. Elisabet has published around 50 peer-reviewed scientific works as well as several book chapters. She supervises PhD students at University of Gothenburg, and at Lund University.
Abstract:
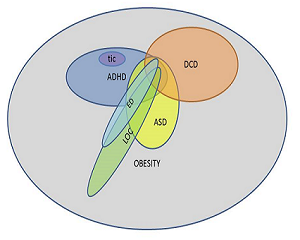
- Statement of the problem: Eating disorders are overrepresented in adults with obesity, but little is known about children with obesity. Attention-deficit/hyperactivity disorder (ADHD) is more prevalent in children with obesity. Impulsive and disorganized behavior, typically for ADHD, may contribute to an eating pattern that initiates weight gain, and complicates the conventional treatment of obesity. No studies on individuals with obesity have investigated the occurrence of autism spectrum disorder (ASD). Little is known about the overlap between eating and neurodevelopmental disorders in children with obesity. The purpose of this study is to investigate the prevalence of eating disorders, ADHD, ASD and other neurodevelopmental disorders in children and adolescents with obesity, and to explore a possible overlap between eating and neurodevelopmental disorders. Methodology: Seventy-six children (37 girls, 39 boys) were recruited at referral to a university outpatient clinic. The parents were interviewed regarding the child’s psychiatric morbidity and completed parental questionnaires pertaining to ADHD, ASD and other neurodevelopmental disorders. The parents were screened for adult ADHD. The probands completed instruments pertaining to eating disorders. Anthropometric and metabolic data were collected. Findings: Body mass index ranged between SDS 1.92 and 5.90, and age between 5.1 and 16.5 years. ASD or ADHD was diagnosed in 13.2 % and 18.4 % of the children, respectively. Twenty-five per cent were screen-positive for motor problems, 31.6 % had at least one neurodevelopmental disorder. 18.4 % had a parent who screened positive for adult ADHD. DSM-5 eating disorders were rare but so-called “loss-of-control eating (LOC)” was present in 22 % of the adolescents. One in three with LOC had also a neurodevelopmental disorder. Conclusions & Significance: ASD and ADHD are overrepresented in clinical populations of children and adolescents with obesity. ADHD and LOC both reflect how impulsive traits can manifest in obese children.
Cristiana Pop
Bucharest University of Economic Studies, Romania
Title: Physical (in) activity - physical and psychological effects
Time : 14:55-15:20

Biography:
Cristiana Pop is currently teaching as full professor in Bucharest Economic Studies University. She has her expertise in teaching physical education in higher education and training athletics mainly for university contests. Her main research interests are in education quality and social issues related with health, physical activity, eating behaviours and wellbeing. She authored “The role of physical activity in promoting well-being” (2015), Athletics for Students (2013) and other few books promoting physical activity and a healthy lifestyle. She is member of The Romanian Agency for Quality Assurance in Higher Education, member of Romanian Athletic Federation (Women Commission) and has research collaboration with Romanian Academy Anthropological Institute Research Center. She is serving as senior editor and member in the editorial board of several reviews in education, health and sport sciences domain.
Abstract:
The globalization of overweight and obesity, the acute perception of being stressed most or all the time, the sedentary life style and the comorbidities of those behaviours might be the most comun consequences for the new millenium generation and their families. Education and healthcare systems are attempting a weak counterattack to this aggressive epidemic and to the consumption culture which pushes the younger generation towards a greedy lethargy. If 5 years ago we were worried because physical activity among European children tends to drop significantly between the ages of 11 and 15 years and only 20% of them exercise regularly, nowadays it is certain that physical inactivity accounts for more than 5 million deaths each year globally. The obsessive informatic and communication technology use results in a progresive physical skills decay and less social interaction. Today when the inteligent phones are shaping our daily life, our bodies are also shaped by bending the neck and back in a „tapping position.” A bad posture has not only physical consequences, but psychological also: an upright, open, expansive posture is associated with power, self confidence and good mood. There is a significant correlation between self body image perception and self esteem, mediated by weight and subsequent by fat deposits. Results indicates a consistent statistically significant correlation between body mass index and body dissatisfaction (r (158) = 0.56, p< .0005), with a prevalence of 79% of body dissatisfaction on young women. Integrating physical and health education in overweight preventative strategies would have effect in reducing the occurrence of physical and emotional disorders and co-morbidities associated with these later, over the lifetime.
Hsien-Wen Kuo
National Yang-Ming University, Taipei, Taiwan,
Title: Association of the availability of maternal and child health center (Posyandu) with child weight status in Indonesia: a cross-sectional study
Time : 16:05-16:30

Biography:
Thomas Kuo has completed his PhD at the age of 30 years from Taiwan University and worked as visiting scholar at UC Berkeley. He is the professor in National Yang-Ming University and he has published more than 200 papers in reputed international and domestic journals and has been serving as an editorial board member of repute.
Abstract:
The Indonesian government has focused on improving Maternal and Child Health (MCH) through the organization of volunteer-staffed Integrated Health Service Post (Posyandu). However, little is known about the childhood obesity prevention practices of MCH in Indonesia or their equivalent counterparts in other countries. The present study aims to assess the association of the availability of Posyandu with child weight status and what factors might influence such associations. This was a secondary analysis of data collected in the 2013 Riskesdas (or Basic Health Research) survey, a cross-sectional, nationally representative survey of the Indonesian population. Height and weight, information regarding the availability of Posyandu, and basic characteristics of the study population were collected from parents with children aged 0 to 5 years (n = 63,237) in 2013. Non-availability of Posyandu significantly raised the odds of being obese (OR=1.13, p<0.01). However, non-availability of Posyandu did not seem to show a significant relationship in the odds for overweight. This relationship persisted after a full adjustment. There was effect modification by household wealth of the association between the availability of Posyandu and child weight status. The availability of Posyandu has a protective association with child obesity in Indonesia. Household wealth modified this association. MCH services are well placed to play an important role in obesity prevention in early life.
Odds ratio and adjusted odds ratio (95% CI) using multinomial logistic regression model for overweight or obesity compared to normal weight according to maternal and child health
- Sessions: Childhood Obesity | Child Nutrition | Childhood Obesity Prevention | Behavioral & Environmental Factors | Economic costs of overweight and obesity | Bariatric surgery for obesity and metabolic disorder

Chair
Fatemeh Rabiee
Birmingham City University, UK

Co-Chair
Lenwood W Hayman
University of Michigan – Flint, USA
Session Introduction
Ellie Wright
EGW Research Institute LLC, USA
Title: Deficiency in Vitamin D and Calcium and the associated comorbidities in overweight children
Time : 11:45-12:10

Biography:
She graduated with Summa Cum Laude, Bachelor of Arts from Arizona State University. In 2010, she received a Master Degree from ASU and a Certificate of Geriatric and Gerontology from University of Arizona. In 2015, she obtained a Doctoral Degree in Naturopathic Medicine from Southwest College of Naturopathic Medicine, Tempe, Arizona.
Abstract:
Obesity is increasing in epidemic proportion around the world with most concern for health issues among children. Vitamin D (25OHD) deficiency is reported world wide. Low 25OHD levels are associated with dyslipidemia and insulin resistance with increased risk of cardiovascular complication in adulthood. Studies suggest that a low vitamin D which is linked to dysregulation of white adipose tissue and that calcium influences adipocyte metabolism. Dietary Calcium has been also shown to increase faecal fat excretion. Deficiency of vitamin D in children is linked with further comorbidities in life such as hypertension, myocardial infarction, and stroke, as well as other cardiovascular-related diseases, such as diabetes associated with impairment of cooperative signalling from the 1,25-(OH)(2)D(3)-activated vitamin D receptor (VDR). Vitamin D and calcium insufficiency causes cellular dysfunction in many organs and could increase the risk of diseases, particularly of osteoporosis, colorectal and breast cancer, inflammatory bowel disease, insulin-dependent diabetes mellitus type I, metabolic syndrome, diabetes mellitus type II, hypertensive and cardiovascular disease. This research focuses on the mechanisms by which calcium and vitamin D could help regulate body weight and might be able to prevent comorbities in overweight children.
Naguib Abdel Reheim
University Hospital - Sharjah ,UAE
Title: Weight Awareness among Parents and Health Care Providers in Sharjah, UAE
Time : 12:10-12:35
Biography:
Dr. Naguib has many years of clinical experience in paediatrics. He has contemporary experience in the management of young children and teenagers with endocrine disorders specially childhood diabetes and obesity, including modern therapeutic interventions like insulin pump and continuous blood glucose monitoring.
Dr. Naguib also runs a general paediatric clinic that deals with common paediatric problems like fever, asthma and common respiratory problems, vaccinations, common gastrointestinal disorders, follow up of nutrition, growth and development.
Dr. Naguib’s professional experience also includes academic appointments with the University of Sharjah, UAE, as an Assistant Professor of Paediatrics in the College of Medicine and Health Sciences. He is also the chairman of the hospital CME Committee at UHS and provides leadership, coordination and direction to both internal and external CME programs.
Abstract:
Background:
Overweight/obesity is common in UAE as in many parts in the world. Management of obesity in children is usually not rewarding because of many barriers. Prevention of obesity is therefore of priority importance. Proper weight perception and awareness among parents and health care providers are basic prerequisites to achieve this aim
Objectives:
This study looks at weight perception among parents and health care providers in Sharjah, UAE
Methods:
Retrospective review was done for 1000 patients files aged 2 to 18 years who visited UHS pediatrics OPD during 2015. Purpose of the visit, diagnosis of weight status, documented general and specific weight counseling in cases of overweight/obesity were reviewed. Overweight and obese are defined as > 85th and >95th centiles respectively based on CDC BMI chart
Conclusions:
1-Most of parents in UAE have weight misperception and are unaware of overweight/obesity as a medical disease
2-Many paediatricians also have weight misperception; they care for weight issue only if the patient visit is for weight abnormality, even in cases of obesity.
3-Weight counselling in children with normal weight is not a routine practice among most physicians
4- Weight misperception of parents and physicians can be a significant barrier for obesity prevention programme.
5-Health education of parents and training of physicians for weight counselling for all children visiting OPD is recommended for obesity prevention.
Ellie Wright
EGW Research Institute LLC, USA
Title: Topic: Childhood obesity: the relations between fatty acids, gut microbiota and low grade inflammation
Time : 12:35-13:00

Biography:
Ellie Wright graduated with Bachelor of Arts (Summa Cum Laurea) from Arizona State University. She obtained a Master Degree from Arizona State University and a Graduate Certificate in Geriatric and Gerontology from University of Arizona. In 2015, she received a Doctoral Degree in Naturopathic Medicine from Southwest College of Naturopathic Medicine, AZ, USA. She is a passionate researcher in natural medicine, prevention and cure.
Abstract:
The purpose of this research is to analyze if low grade inflammation in obese children could be address with probiotics/prebiotic and fatty acids as they play a role in intestinal permeability, intestinal inflammatory responses and regulating insulin and fat storage. Recent evidence suggests that gut microbiota is involved in the control of body weight, energy homeostasis, inflammation and plays a role in the pathophysiology of obesity. Obesity in children is characterized by low grade inflammation expressed by proinflammatory cytokines, adipokines and reactive oxygen species. With the increased usage of antibiotics and refined foods there is an increased alteration of microbiota done via several mechanisms: increasing gut permeability with subsequent metabolic inflammation, impairing short-chain fatty acids synthesis, and altering bile acids metabolism. Probiotics/prebiotics affect the gut microbiota directly and indirectly by modulating its bacterial content and through bacteriocins. Long-chain saturated fatty acids are associated with dysbiosis while short-chain and certain unsaturated fatty acids, protect against dysbiosis and possible may promote insulin sensitivity and regulate energy metabolism. This research aims to find nutritional approaches for preventing and attenuating the pathological consequences of obesity in children.
Vered Kaufman-Shriqui
Ariel University ,Israel
Title: Improvement in bagged lunches following an intervention in the preschool setting: a randomized controlled trial
Time : 14:10-14:35

Biography:
Vered Kaufman-Shriqui is a registered dietitian and an epidemiologist. She received her M.Sc. in nutrition (with honors) from the Hebrew University, and her Ph.D. in Epidemiology from Ben-Gurion University, Israel.
Dr. Kaufman-Shriqui is a faculty member in the Department of Nutritional Sciences in Ariel University. She has conducted several intervention trials aimed to reduce childhood obesity, and examined the association of social determinants with maternal chronic conditions. During her research she focused in developing culturally adopted methods to collect nutritional information.
Her current research focuses in the effect of social capital and food policies on body weight and food choices.
Abstract:
More than a third of preschool children's nutritional intake is consumed during school hours. However, few studies have assessed the quality of bagged lunches sent from home to feed children during the day. A cluster-randomized controlled-trial examining the effect of a preschool-based comprehensive intervention on nutrition behaviors among low socioeconomic status (LSES) preschool-aged children was performed. During a full school year, LSES preschoolers (mean age 63m, 48% boys) and their mothers were recruited from preschools in a large town in Israel and cluster-randomized to an intervention group (7 preschools, 184 children) or to a control group (4 preschools, 74 children). The intervention children received in school, nutrition education and physical activity (PA) classes; intervention parents and teachers received healthy nutrition classes. The control group received PA classes for children only. Family data were obtained by parental interviews. Food and nutrition knowledge testing and observations and anthropometric measurements were conducted at baseline, at intervention termination and at the end of the school year. Differences between groups were analyzed while controlling for clustering. Of the 258 children enrolled, 220 (87.6%) completed the six-month program. Improvement in the quality score of bagged lunches was shown in the intervention group (p<.0001). Intervention group increased fruit and vegetable consumption and habitual water drinking (p=0.02), and decreased sweet-drinks consumption (p=0.05). In this study, the bagged lunches prepared at home and sent with the children to their preschools reflected marked changes in parental feeding behaviors. The six-month follow-up showed that this improvement was sustained.
Carmina Niña Salac-Grantoza
University of Santo Tomas Hospital, Manila, Philippines
Title: The Validation of an Instrument to Assess Parental Feeding Styles of Children in Filipino Language
Time : 14:35-15:00

Biography:
Carmina Niña R. Salac, M.D. has completed her degree in Doctor of Medicine in the University of Santo Tomas, Manila, Philippines, in 2011. She completed her residency in Pediatrics in University of Santo Tomas Hospital, Manila in 2015. She is currently a fellow-in-training of Pediatric Critical Care Medicine in the same hospital.
Abstract:
Overweight and obesity are emerging major problems among children today worldwide. Research on parent feeding styles and practices has begun to provide some clues about the role parents play in the etiology of childhood obesity. Only recently has attention been directed toward the parental feeding styles. Experts have suggested that gestation to early infancy is a critical period in which physiologic changes occur that greatly influence a child's later risk for obesity. The objective of the study is to examine validity and reliability of an instrument translated to Filipino language for characterizing parental feeding practices. Subjects were the parents with toddlers from the University of Santo Tomas Hospital. A Focus Group Discussion was done. The Toddler Feeding Questionnaire was translated to Filipino language. A final questionnaire underwent pretesting and Cronbach’s alpha test. Data analysis was done using Strata SE version 13. Quantitative variables were summarized while qualitative variables were tabulated. Test-retest and Cronbach’s apha tests were done. A total of eighteen (18) parents participated in the study. About 89% of the toddlers had normal weight according to the WHO growth standards (weight for length). All but two (2) items (Q18 and Q33) in the final questionnaire reached significant differences (p <0.05). The overall internal reliability of the questionnaire was acceptable (alpha = 0.82). This instrument was found to be valid with acceptable reliability and internal consistency.
Lucia Pacifico
Sapienza University of Rome, Italy
Title: Thyroid function in childhood obesity and metabolic comorbidity
Time : 15:00-15:25

Biography:
Prof. Lucia Pacific Pediatrics Assistant Professor of Sapienza University of Rome;
Currently Professor holds the position of Executive Level I and Head of Pediatric Infectious Diseases and Hepatology in the Department of Pediatrics and Child Neurology, Azienda Policlinico Umberto I, Rome.
Her research interest are: Pediatric Hepatology (cholestasis, jaundice, metabolic diseases of the liver); Fatty liver in children; Nutrition; Markers of inflammation and cardiometabolic risk in children with visceral obesity; Pediatric Gastrointestinal infections
Lucia Pacifico graduated in Medicine and Surgery (1977) at the University "Sapienza" of Rome with honors, specializing in Pediatrics (with honors), with specialization in Neonatology with honors at the "Sapienza" University of Rome.
Her later obtained a degree in Medicine and Surgery recognized in the United States (Educational Commission for Foreign Medical Graduates - 1979; Visa Qualifyng Examination- 1980).
Her holds the License to a doctor surgeon recognized in the United States (Board of Medical Examiners - 1982).
Abstract:
Childhood obesity is a worldwide health problem and its prevalence is increasing steadily and dramatically all over the world. Obese subjects have a much greater likelihood than normal-weight children of acquiring dyslipidemia, elevated blood pressure, and impaired glucose metabolism, which significantly increase their risk of cardiovascular and metabolic diseases. Elevated TSH concentrations in association with normal or slightly elevated free T4 and/or free T3 levels have been consistently found in obese subjects, but the mechanisms underlying these thyroid hormonal changes are still unclear. Whether higher TSH in childhood obesity is adaptive, increasing metabolic rate in an attempt to reduce further weight gain, or indicates subclinical hypothyroidism or resistance and thereby contributes to lipid and/or glucose dysmetabolism, remains controversial. My report will highlight (1) current evidence on thyroid involvement in obese children and discusses the current controversy regarding the relationship between thyroid hormonal derangements and obesity-related metabolic changes (hypertension, dyslipidemia, hyperglycemia and insulin resistance, nonalcoholic fatty liver disease) in such population; (2) the possible mechanisms linking thyroid dysfunction and pediatric obesity; and (3) the potential role of lifestyle intervention as well as of therapy with thyroid hormone in the treatment of thyroid abnormalities in childhood obesity.
Ata pourabbasi
Tehran University of Medical Sciences, Iran
Title: Obesity or normal nutritional behavior; which should be the main focus in children and adolescents?
Time : 15:25-15:50

Biography:
Ata Pourabbasi entered to medical school at Tehran University of Medical sciences at 1999. He continued his education at endocrinology & Metabolism Research Institute (EMRI) and earned his PhD in the field of cognitive neuroscience. His main research focus is relation between health problems, medical illnesses and cognitive functions especially in children and adolescents. He has developed a new concept named “COGNITOMICS” in this regard in which human behavior is considered as the main window into cognitive functions. He has established Cognitomics Lab at EMRI for expanding his studies in this issue.
Abstract:
Over the past decades, obesity have become a global concern. This issue not limited to a certain range of age so that a plethora of research body has focused on obesity in childhood and adulthood. Several studies have also supported the impact of obesity in raising the rate of mortality and the incidence of non-communicable diseases such as cancer and cardiovascular diseases. However, in parallel with these findings, a new concept, metabolically healthy obesity has been developed in this area. According to this new concept, metabolic parameters could be normal such as insulin resistance, lipid profile, etc. despite of obesity phenotype. Consistently, it has been confirmed in several studies that metabolically healthy obese individuals are not significantly different from those of normal weight in respect of risk of obesity-related disorders such as CVDs, and liver fibrosis.
Putting all these findings together raises the question whether the obesity phenotype is a troublemaking health issue or obesogenic behaviors even without obesity phenotype? Is it possible for obese individuals to have normal behavior, and normal weight individuals, in contrast, have inappropriate behaviors such as excessive intake of junk foods, sedentary life style, overeating, etc? Although, no documented study has been so far carried out in this field, but the experience of the author attest to the fact that the obesity phenotype is not necessarily correlated with the eating behaviors; and the issue which leads to the obesity-related complications in different ages maybe not the obesity phenotype but is the abnormal nutritional behaviors even though in non-obese individuals. Thus, it seems necessary to put more emphasis on establishing normal nutritional behaviors in childhood instead of obesity phenotype and fitness.
Ievleva Kseniia
Scientific Center for Family Health Problems and Human Reproduction ,Russia
Title: No association between LEPR Q223R and plasma leptin level in Caucasian female adolescents

Biography:
Kseniia Dmitrievna Ievleva finished the faculty of medical biochemistry of Irkutsk State Medical University in 2014. On summer 2015 she got the certificate of doctor of laboratory. Now she is a postgraduate student in Scientific Centre for Family Health Problems and Human Reproduction. Her present study aims to examine the role of heredity in the development of obesity in adolescents living in Eastern Siberia.
Abstract:
Statement of the Problem: The hormone leptin are involved in regulation of energy metabolism. Effect of the leptin carried out through binding to its receptor in target tissues. Many polymorphisms of LEPR gene were found out including Q223R (Gln223Arg). This polymorphism produces molecular changes in extracellular region of the LEPR. Several studies showed the association this polymorphism with obesity and leptin level in adult and adolescent samples. However, some studies showed no this association. Methodology & Theoretical Orientation: A total of 128 Caucasian female adolescents living in Eastern Siberia (Irkutsk city, Russia) were observed. 59 of them were included in control group (average age 15,72±0,93; SDS BMI 0.84±0.55) and 69 adolescents with overweight and obesity was in main group (average age 16,04±1,07; SDS BMI 2.52±0.72). Plasma leptin level (PLL) was determined using commercially available enzyme-linked immunoabsorbent assay (LEPTIN ELISA kit, DBC, Canada) with an absorbance microplate reader MultiSkan ELX808 (Biotek, USA). Genomic DNA was extracted from EDTA-treated whole blood by commercial kits (DNA-Sorb-B, AmpliSens, Russia). Genotyping LEPR Q223R was performed using polymerase chain reaction (Eppendorf Mastercycler Gradient PC, Germany) with electrophoresis detection. Statistical analysis was performed by soft “STATISTICA8.0”. Findings: The plasma leptin level was significantly higher in main group (50,57±16.06) than in control group (23.91±14,13) (p<0.001). G-allele frequency was 43.1% in control and 40% in main group (Ñ€=0.862). Comparisons of the meaning circulating leptin levels stratified by LEPR Q223R genotype are showed in Table 1. We didn’t find significant differences of leptin level between carriers of AA, AG and GG genotypes in both groups. Conclusion & Significance: Thus, The plasma leptin level is increased in female adolescent with overweight and obesity. There is no significant association of LEPR Q223R with plasma leptin level and obesity in Caucasian female adolescents living in Eastern Siberia.
Lori Sanderson
Loma Linda University ,USA
Title: Overweight and Obesity Barriers and Facilitators Literature Review

Biography:
Lori Sanderson completed her Doctoral degree in Public Health Education and Promotion. She also holds a Master’s degree of social work and is currently a Licensed Clinical Social Worker. She has worked as a Medical Social Worker for over 12 ½ years now and specializes with children and adolescents who have been diagnosed with kidney disease, diabetes, and craniofacial disorders. She has developed several different programs to help the children with whom she works with to develop healthy coping skills, master the English language, and to lose weight. She is currently working with children and adolescents with kidney disease to lose weight. She also has experience working with clients with eating disorders.
Abstract:
Over eighty nine percent of children with type 2 diabetes were considered obese or overweight (Liu, Lawrence, Davis, et al 2009). Childhood obesity is associated with an increased risk of kidney disease and mortality of kidney disease (Wang, Chen, Klag, & Caballero 2006). Patient education is not sufficient to motivate this population to increase their physical activity and healthy eating. Without identifying the barriers to successful weight loss or successful increase in physical activity and healthy eating, this population will remain stagnant. The purpose of this article is to identify the barriers of physical activity and healthy eating for patients with kidney disease or diabetes. A systemic literature review was conducted to identify the barriers of weight management for children and adolescents with kidney disease or diabetes. Upon identifying the barriers, the facilitators, which aim to improve health, can be established. Studies were found using pubmed, academic search premier, and the global internet. Search criteria included obesity rates, physical inactivity rates, unhealthy eating, risk factors for children to acquire diabetes or kidney disease, barriers to healthy eating, barriers to healthy eating and exercise. Although not all of the barriers were from research studies of patients with kidney disease or diabetes, there were multiple barriers which occurred in more than one study, which will be discussed later. Patient education alone isn’t sufficient to increase physical activity and healthy eating. Investigators need to understand what prevents the population from increasing their physical activity and healthy eating, so that they can develop and test potential solutions (facilitators). More research is needed to identify barriers among specific populations such as children with diabetes or kidney disease, and to understand why many of the barriers differ among various populations. More research is also needed to identify and test facilitators to healthy eating and physical activity.
Rana Saleh
Knowledge to Policy Center, AUB, Lebanon
Title: Promoting Effective School Policies for Childhood Obesity Prevention in Lebanon through Advocacy, Citizen Engagement and Knowledge Translation

Biography:
Rana Saleh is a licensed dietitian and public health practitioner. In 2013, she graduated with a Bachelor degree in Nutrition and Dietetics from Beirut Arab University and earned Jamal Abdul Nasser Award for Academic Excellence. Then she completed a master degree in Public Health at the American university of Beirut in 2016 and was inducted to the honorary society of public health, the Delta Omega. She is currently the advocacy officer at the Knowledge to Policy- K2P Center at FHS-AUB working on launching the advocacy and citizen engagement arms in the center. Her current work also revolves around NCD prevention including youth alcohol consumption, childhood obesity, tobacco, and other projects.
Abstract:
Background: Child overweight & obesity (COO) in Lebanon has reached alarming levels of 34.8% & 13.2% respectively. With one of the highest percentages in the Eastern Mediterranean region, COO in Lebanon increased by approximately two folds in the past decade, without policies for prevention, despite mounting evidence of their effectiveness. This study examines the use of citizen engagement, advocacy & knowledge translation (KT) tools & platform in the uptake of research evidence on effective school policies in COB prevention.
Methods: The following work was conducted & evaluated: 1) development of a policy brief for effective school policies for COO prevention in Lebanon, 2) Citizen Consultation (CC) meetings using innovative data visualization (IDV), 3) a national Policy Dialogue (PD),
4) implementation of an advocacy framework. Results: The policy brief: Synthesizing high quality international & local evidence along with key informant interviews resulted in identifying 3 major effective elements for a comprehensive school policy solution. The CC & PD: Those elements were discussed in both dialogues for consensus & identifying key implementation considerations using IDVs. Furthermore, the participants in the CC thought that it can affect decision makers (70%), allow joint decision making (70%) and almost all wanted to be involved in further advocacy efforts. The advocacy framework: a framework was developed & piloted over the course of the implementation of the policy elements. Conclusion: School policies for COO prevention are effective but require using an integrated KT approach to bring a change in policy & practice. That entails engaging citizens in the decision-making & implementing evidence-informed advocacy strategies & coalitions to influence actions along with using KT tools and platforms. Citizen engagement strategies empower citizens to be involved in the decision- making process & in enhancing accountability & advocacy in health policy. Study findings will inform similar work in other countries.
Michelle Queally
JE Cairnes School of Business and Economics, Ireland
Title: Maternal perception of weight status in young Irish children

Biography:
Michelle is currently employed as a Health Research Board post-doctoral research fellow. She holds a PhD and a Masters in Health Economics. Her research activity and interests are in the economics of childhood obesity and complex public health interventions including behavioural change. Michelle is also interested and actively researching economic outcome measurement in children. Her work to date has involved the application of mixed methods, discrete choice experiment and economic evaluation techniques to explore a variety of questions pertaining to the economics of obesity. The output from this work, which has involved collaboration with colleagues across multiple disciplines, has been published in a number of leading national and international peer-reviewed journals. Prior to joining the Health Behaviour Change Research Group in 2016, Michelle was a recipient of the Irish Research Council Scholarship and also the Hardiman Scholarship Michelle was a Visiting Scholar at Cornell University, New York, 2016
Abstract:
Statement of the Problem: The childhood obesity epidemic requires a sense of urgency and new avenues for prevention focused on the first 5 years of life (Burns et al., 2011). Parental perception of early childhood weight is an important concept. Parents can shape early eating and physical activity patterns in their children (Lindsay et al., 2006). If parents are unable/unwilling to recognize that their child is at risk for overweight, they cannot intervene early to prevent further excess weight gain. Furthermore, if perception influences the use of parental feeding practices (Hager et al., 2012), particularly a perception that is incorrect, parents may inadvertently employ practices that facilitate the development of overweight/obesity in their child. Understanding parental weight perception within this age-group during a time that reveals great potential for obesity prevention is of great importance. Methodology & Theoretical Orientation: Using the infant cohort data (wave 2 and 3) of the Longitudinal Growing up in Ireland (GUI) study, (children aged 3 and 5 respectively), we aim to examine firstly, if there is evidence of parental weight misclassification within this cohort. Next, the factors associated with the inaccuracy (if any) of parental perception of the child's weight are examined (e.g. parental education and younger parents). Finally, we observe if parental misclassification alters as the child gets older (that is from age three to age five). Estimating the marginal effects using probit models, the results indicate a notable lack of awareness in Irish mothers of overweight 3–5 year olds about their children’s weight status, more so for mothers of 3 year olds (wave 2). Findings: Across both waves, children whose mother is overweight or obese are more likely to misclassify their child’s weight. outstanding issues. Conclusion & Significance: Before early childhood specific behavioural interventions can be developed and tested, additional research examining techniques to influence parental perception are needed.
Oparaocha Evangeline Tochi
Federal University of Technology, Nigeria
Title: Childhood Obesity in Nigeria: Causes and Suggestions for Control

Biography:
Rev. Sr Prof. Evangeline Oparaocha, is a professor of public health parasitology, of the Department of Public Health, Federal University of Technology, Owerri, Nigeria. She is highly skilled in diverse aspects of public health and has contributed tremendously in areas of epidemiology, prevention and control of major endemic parasitic diseases, use of ethnobotinicals in the control of endemic diseases, gender disparity in disease burden, community participation in disease control, prevention and control of highly, prevalent non-communicable diseases as well as occupational and environmental health and safety. With her tremendous, imperative research skill and over 19 years of teaching experiences in universities, she has played a leading and unparallel role in championing and repositioning high quality teaching and research techniques in the department. She has mentored numerous undergraduate and postgraduate students whose researches and health outreaches have positively affected the health outcome of communities around and beyond. Her researches have translated into more than 40 quality international journal articles in various aspects of public health, minor productive works and books in other disciplines. She has made a global mark in the control of tropical diseases using ethnobotinicals. Besides her academic field, she scripts and produces home video films.
Abstract:
Childhood obesity is fast becoming a global public health concern, not only because of increased BMI but majorly due to attendant health consequences. While it is expected that childhood obesity affects only developed, affluent countries, the current trend shows a gradually shift in dimension towards low income, developing countries like Nigeria. Although, causes of obesity differ intrinsically among nations, the health outcomes appear to be similar, which include, renal, cardiovascular, musculoskeletal, respiratory and neurological disorders, as well as psychological and emotional problems. Identified causes in Nigeria include among others, shift in life style and behaviour, medication, cultural beliefs, taboos, food habit and choices as well as genetic makeup of individuals. Suggested approaches towards control would include timely intervention, health education, life style modification, shift in bogus beliefs and taboos, as well as change in food habit and food preferences. The roll of parents and the media in the control of childhood obesity will also be highlighted.
- Food and Nutrition | Behavioural & Environmental Factors | Childhood Obesity Prevention | Thyroid and Obesity
- Young Researchers Forum
Session Introduction
Elaine Shea
University of Chester , Ireland
Title: The effectiveness of the ‘Way to Go Kids’ programme for children who are overweight and underactive
Time : 16:35-16:55

Biography:
Elaine Shea has her expertise in Exercise and Nutrition Science graduating with her Master’s Degree from the University of Chester in 2016. She received a distinction in her Masters project titled ‘The effectiveness of the ‘Way to Go Kids’ programme for children who are overweight and underactive. As a Sports Development Officer for the Limerick Sports Partnership she redesigned the ‘Way to go Kids’ programme and manual along with the Limerick Health Service Executive which was adapted from an American programme to meet the needs of Irish children. The Irish ‘Way to go Kids’ was published in October 2015 and is the first National programme to target overweight children and childhood obesity.
Abstract:
Childhood overweight and obesity has become an epidemic health issue in today’s society with one in four children (9, 7 and as young as 3 years of age) are overweight or obese in Ireland. The cost of treating obesity in Ireland is costly and has a huge economic impact. ‘Way to go Kids’ is a nutrition and fitness education programme designed to support overweight children in developing the skills needed to adopt a healthy lifestyle. ‘Way to go Kids’ was adapted from an American programme and redesigned by the author from Limerick Sports Partnership and by Limerick Health Service Executive to meet the needs of Irish children. The Irish ‘Way to go Kids’ is the first National programme to target overweight children and childhood obesity in Ireland. This report is the first review of the effectiveness of the Irish ‘Way to go Kids’ programme. Methodology & Theoretical Orientation: 24 overweight/obese children (9-12years) and their parents were recruited for this study. Twelve participants weight and fitness levels before and after the ‘Way to go Kids’ programme were compared to twelve participants of a similar stature in a control group who did not participate in the programme. Pre and post questionnaires were also carried out to investigate if the 'Way to go Kids' programme improves participants' knowledge, confidence, attitudes and behaviours in relation to nutrition, physical activity and weight. Findings: Results revealed that participants who completed the ‘Way to go Kids’ programme lost weight, decreased waist circumference, decreased BMI, improved muscle strength, muscular endurance, cardiovascular endurance, lung capacity and flexibility. ‘Way to go Kids’ Participants also showed an increase in knowledge and confidence, and positive changes in attitude and behaviours in relation to nutrition, physical activity and weight. Conclusion & Significance: Due to the small scale of this study some of the results did not reach statistical significance. However, indication of clinically different changes were identified which may have become statistically significant if the study had continued for a longer timeframe.
Rabab Alkutbe
University of Plymouth ,UK
Title: The correlation between socio-economic status and energy and nutrient intake of girls aged 8-11 years in Saudi Arabia
Time : 16:55-17:15

Biography:
Rabab Alkutbe, who is currently a PhD Candidate, examines the relationship between body composition, nutritional intake and physical activity in children. Since she finished her degree in Nutrition and food sciences in Saudi Arabia followed by a diploma in Complementary Medicine (herbal medicine), she perused her life passion, research which led to undertake a master’s degree in public health (Nutrition) in Australia in 2010. She is a highly competent researcher, who can take research through all stages from hypothesis, design and execution of experiments data analysis, became closely involved in the issue of childhood obesity and has intensive experience in aspects of public health. She skilled in the application of various techniques to solve various research questions and has significant experience in a variety of laboratory techniques in the area of nutrition.
Abstract:
Obesity has become a major world-wide health issue. Social and economic factors may influence nutritional intake as a result of differing regional diets, lifestyles and cultures, and these require closer scrutiny. However, this issue has not been examined in studies of children in Saudi Arabia. The aim of this study was to assess energy and nutrient intakes of girls aged 8-11 years in western of Saudi Arabia according to socio-economic status (SES).
Girls (n= 134) participated from different schools (private n= 4 and public n= 3). Height and weight were measured and BMI was calculated. Girls were classified as obese, overweight, healthy weight and underweight according to BMI centile charts (CDC). Dietary intake was measured via a 4-day food diary and with the purpose of assessing the household socioeconomic status as classified by king Khalid foundation (3); parents or carers were asked to fill out a questionnaire attached to the diet diary. Dietary data was analysed using Arab Food Analysis Programme 1st version 2007 analysis package. Data were statistically analysed using SPSS version 21. Number of subjects according to their income status is presented in Table 1. Results showed that 17 out of 28 obese subjects were from high-income families, whereas 7 out of 14 underweight girls were from low-income families.
Nevertheless, chi- square was not significant suggesting that being from any family income status would not affect the BMI status (Chi-Square =5.151- P=0.272). There was a positive correlation between the two variables, r = 0.22, n = 134, p < .0.05, with high levels of energy intake associated with high levels of income as shown in Table 2.
To sum up, results showed that there is a positive relationship between energy intake and the family income status.
- Exercise & Kinesiology | Genetics and Obesity | Child Nutrition
- Video Presentations
Session Introduction
Mehmet Emre Atabek
Necmettin Erbakan University, Turkey
Title: Evaluation of Periaortic Adiposity and Metabolic Disorders in Obese Children
Time : 17:35-18:00

Biography:
Professor Mehmet Emre Atabek has completed his Ph.D. at the age of 37 years from Erciyes University and postdoctoral studies from Selcuk University School of Meram Medicine. He is the director of Pediatric Endocrinology, a premier pediatric endocrinolgy and diabetology service organization. He has published more than 120 papers in reputed journals and has been serving as an editorial board member of repute. He has been interested in searching metabolic problems of obese children in most of his articles. His articles have been cited more than 1100 citations by another article in Web of Science so far. He continues to work as head of the Department of Pedaitric Endocrinolgy, Necmettin Erbakan University.
Abstract:
OBJECTIVE:
To evaluate the relationship between periaortic fat thickness (PAFT) and parameters involved in the development of metabolic complications of the cardiovascular system in obese children and to assess the usefulness of echocardiographic measurements of PAFT in correlation with cardiovascular risk factors.
METHODS:
The study was conducted with 263 obese and 100 healthy children and adolescents. PAFT was measured with echocardiography method which was recently performed in obese children and adolescents.
RESULTS:
PAFT was significantly higher in the obese group (0.258±0.031 mm) than in the control group (0.137±0.032 mm) (p<0.001). In multivariable regression analysis, body mass index-standard deviation score and total body fat were predictors of PAFT. The area under the receiver operating characteristic curve was 0.989 and was quite significant at p<0.001. PAFT above 0.179 mm was determined as the cut-off value in obese children and adolescents (sensitivity=1, specificity=0.97).
CONCLUSION:
The measurement of PAFT in obese children and adolescents may be a good method to reveal the presence of early cardiovascular risk.
Sivapatham Vishnu Kumar
Eastern University, Sri Lanka
Title: Reliability of Body Mass Index in predicting cardiovascular risk factors in overweight and obese children
Time : 18:00-18:25

Biography:
Vishnu Sivapatham is a Researcher with a strong background in Health Science especially in Pediatrics. He has his expertise in Evaluation and passion in improving the health and wellbeing. After completing his MBBS Degree at Eastern University in 2012, he completed Post-graduate Diploma in Child Health in Sri Lanka. Currently, he is pursuing his MD in Pediatrics at Post-graduate Institute of Medicine, University of Colombo, Sri Lanka. He is a Lecturer in Pediatrics at Eastern University, Sri Lanka. He is also a member of Sri Lanka Medical Council (SLMC), Sri Lanka Medical Association (SLMA), Young Scientist Forum (YSF), Perinatal Society of Sri Lanka (PSSL) and Nutritional Society of Sri Lanka (NSSL).
Abstract:
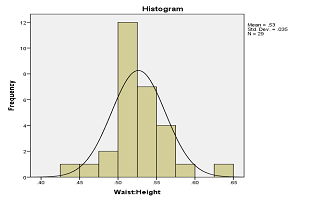
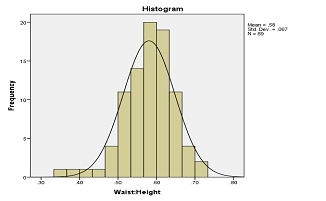
Introduction: Childhood overweight and obesity is in an increasing trend throughout the world. Distribution of body fat is an important determinant in predicting the future cardiovascular risk factors. Body Mass Index (BMI) is the commonly used tool in diagnosing overweight and obesity. Waist circumference (WC) percentile and waist height ratio (WHtR) demonstrated high sensitivity and specificity for detection of abdominal fat mass.
Aim: The aim of this cross sectional study involving children from an urban area, Sri Lankan aged 3-18 years was to investigate the reliability of BMI in predicting central adiposity.
Method: Weight, height, and WC were measured using standard methods and BMI, and WHtR were calculated. The BMI of 85th and 95th percentiles were adopted as cutoff points for overweight and obesity respectively and similar values were considered for WC to define obesity and overweight based on age and sex as per centre for disease control classification. WHtR 0.6 and 0.5 were considered as alert line and action line for interventions respectively.
Findings: Among 116 subjects, 29 (25%) were overweight and 87 (75%) were obese. According to WC percentile 9 (7.7%) were overweight while 107 (92.2%) were obese. Thus BMI has 77.7% (83/83+24) sensitivity and 55.5% (5/5+4) specificity to detect central obesity. The positive predictive value was 95.4% (83/83+4) while the negative predictive value was 17.2% (5/24+5). In our study, 83.7% of actually overweight population lied in alert line (Figure 1) and 43.7% of actually obese population lied in action line (Figure 2).
Conclusion: Even though BMI is a simple tool in detecting overweight and obesity it has low sensitivity and specificity to detect central fat distribution which is more important to predict the future cardiovascular risk factor in children.
Recommendation: Ethnic-specific cutoff value of WC and WHtR will help to identify future cardiovascular risk factors especially in children and adolescents.
- Young Reseacher Forum
